Managing financial operations and achieving sustainability can be complex. From claim denials to coding inefficiencies, even the smallest issue in the RCM process can impact cash flow and create financial strain. Healthcare organizations need accurate, focused solutions that speed up collections and improve yield.
Ovation Healthcare’s revenue cycle management provides full end-to-end or targeted point solutions that improve cash flow, reduce denials, and enhance overall financial performance.
Complete our form to connect with our experts and explore ways we can improve your financial health and achieve sustainable revenue.
Managing financial operations and achieving sustainability can be complex. From claim denials to coding inefficiencies, even the smallest issue in the RCM process can impact cash flow and create financial strain. Healthcare organizations need accurate, focused solutions that speed up collections and improve yield.
Ovation Healthcare’s revenue cycle management provides full end-to-end or targeted point solutions that improve cash flow, reduce denials, and enhance overall financial performance.
Complete our form to connect with our experts and explore ways we can improve your financial health and achieve sustainable revenue.


Ovation’s front-end service is an integral component in healthcare organizations, focusing on the first stages of the revenue cycle process. Ovation’s front end encompasses patient access, patient financial engagement, and coverage identification. With Ovation’s efficient handling of these tasks, we can prevent billing errors and improve patient satisfaction.
Ovation’s mid-cycle service includes charge capture, billing, and optimization. We ensure that all services are accurately documented, coded, and billed according to requirements. By optimizing these processes, Ovation helps increase revenue while reducing the risk of claim denials.
Ovation’s back-end service is the final RCM process, including claims processing and clearing, patient billing and collection, and claims follow-up and collection. Our effective back-end RCM ensures that providers receive timely and accurate reimbursement for their services.

Maximize revenue performance across the full revenue cycle with integrated front, mid, and back-end solutions. From patient access and financial engagement to charge integrity and claims follow-up, Ovation delivers a seamless RCM experience that drives accurate reimbursement, reduces denials, and supports long-term financial health.

Ensure prompt, accurate reimbursement from the start with tech-enabled billing and collections. Our Day 1 approach drives timely claims submission, clear patient communication, and early follow-up to reduce aging accounts, improve cash flow, and deliver a smooth, end-to-end financial experience.

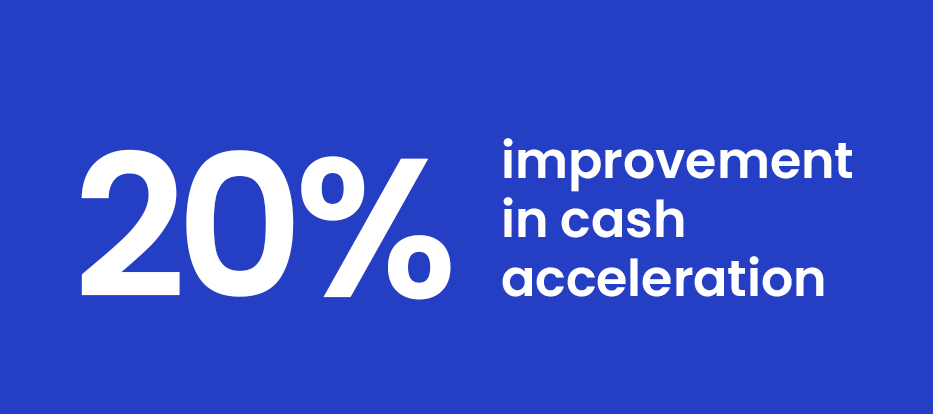
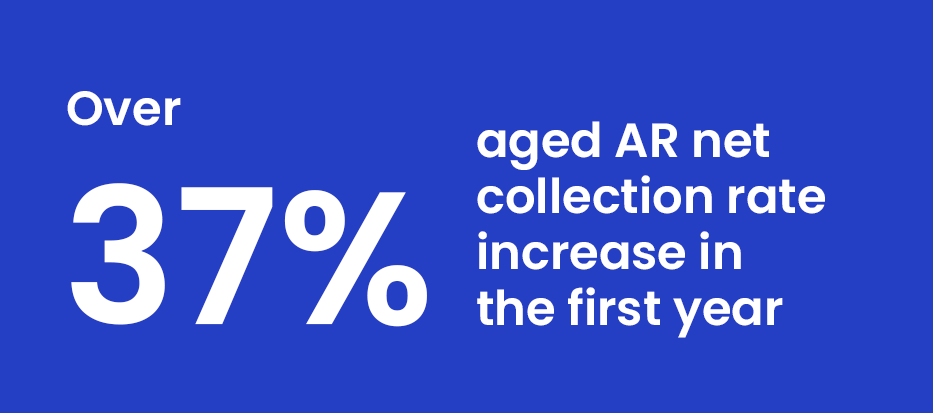
Maximize working capital and reduce aged receivables with cash acceleration and AR spindown strategies. We prioritize high-value accounts, streamline workflows, and focus on fast resolution—boosting revenue recovery and ensuring financial stability across the revenue cycle.

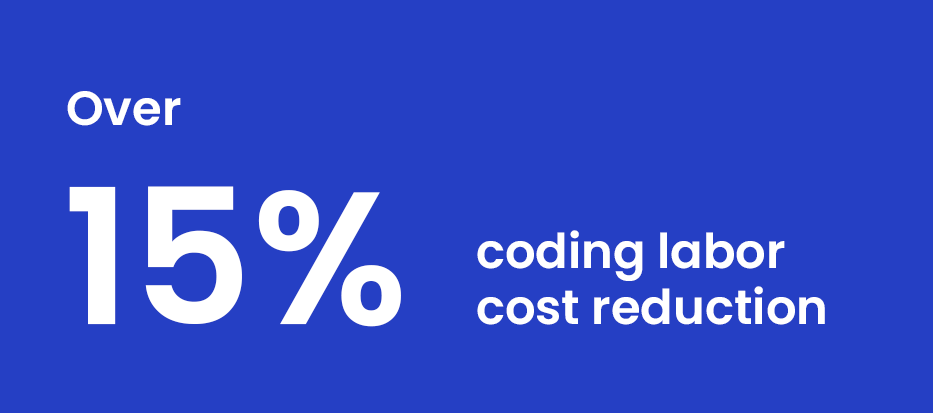
Ensure proper reimbursement and realize revenue opportunities through accurate medical coding. By translating clinical services into clean, compliant claims, coding supports timely payments, reduces denials, and helps hospitals optimize revenue cycle performance.

Strengthen revenue integrity with streamlined ambulatory and professional fee billing. By accurately converting outpatient services into clean claims and timely reimbursements, these solutions help reduce revenue leakage, improve compliance, and enhance the financial experience for both patients and providers.

Strengthen front-end performance with patient access services that support accurate registration, eligibility verification, and financial counseling. By improving data integrity and clarifying coverage early in the process, hospitals reduce claim denials, increase point-of-service collections, and improve patient satisfaction.

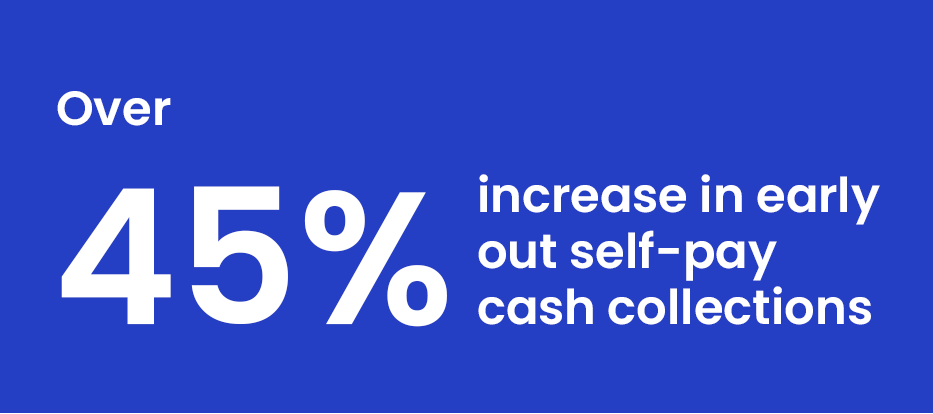
Improve collections and enhance patient satisfaction through early-out services that engage self-pay accounts quickly and compassionately. By combining timely outreach with customized payment plans and digital payment options, this solution accelerates cash flow while easing financial stress for patients.
Resolve payment discrepancies and protect revenue integrity by addressing both claim denials and underpayments. Our targeted review process identifies root causes, appeals denied claims, and recovers missed reimbursements to improve yield and reduce avoidable revenue loss.

Maximize revenue and uncover missed opportunities through comprehensive zero balance account reviews. By analyzing fully paid claims, identifying underpayments, and correcting systemic issues, this process supports accurate reimbursement and strengthens financial performance across the organization.
Ovation offers practical insights that help you improve your hospital’s revenue cycle by making informed decisions to boost efficiency, realize revenue opportunities, and ensure a seamless experience.
Ovation’s provides seamless billing, payment, and insurance handling for your patients, enhancing their experience and creating a more supportive healthcare journey.
Ovation’s expertise spans every stage of your revenue cycle to create scalable solutions that fit your organization’s specific needs.
Ovation’s automated processes help streamline your operations, to manage reimbursement costs and achieve scale, ultimately contributing to strengthened financial health.
Ovation Healthcare is a trusted leader in end-to-end revenue cycle management, helping hospitals realize revenue opportunities, accelerate cash flow, and reduce the cost to collect.
With more than 45 years of experience, we’ve continually refined our approach to deliver scalable RCM solutions that improve financial performance while enhancing both patient and provider experience.
Ovation Healthcare is a trusted leader in end-to-end revenue cycle management, helping hospitals realize revenue opportunities, accelerate cash flow, and reduce the cost to collect.
With more than 45 years of experience, we’ve continually refined our approach to deliver scalable RCM solutions that improve financial performance while enhancing both patient and provider experience.
With over 45 years of experience, Ovation Healthcare delivers industry-leading revenue cycle management solutions and financial advisory services to strengthen and sustain hospitals and health systems nationwide.
We support more independent hospital organizations than any other firm in the nation, providing trusted reimbursement guidance, performance improvement strategies, and scalable RCM support. Our services deliver:
With over 45 years of experience, Ovation Healthcare delivers industry-leading revenue cycle management solutions and financial advisory services to strengthen and sustain hospitals and health systems nationwide.
We support more independent hospital organizations than any other firm in the nation, providing trusted reimbursement guidance, performance improvement strategies, and scalable RCM support. Our services deliver:
Ovation’s assessments, remediation, continuous improvement, and reporting insights are all connected processes that collectively strive to elevate your hospital’s RCM performance and quality through a data-driven approach. Each element builds upon the other, providing your team with a comprehensive view to make informed decisions.
Ovation’s assessments, remediation, continuous improvement, and reporting insights are all connected processes that collectively strive to elevate your hospital’s RCM performance and quality through a data-driven approach. Each element builds upon the other, providing your team with a comprehensive view to make informed decisions.

Ovation is dedicated to your financial health and the well-being of your patients. Our proven track record, innovative solutions, and commitment to excellence make us the trusted choice for your RCM services. Whether through full end-to-end RCM or point solutions, we are committed to vitalizing your financial performance so that you can focus on the provider experience and patient care.
Ovation is dedicated to your financial health and the well-being of your patients. Our proven track record, innovative solutions, and commitment to excellence make us the trusted choice for your RCM services. Whether through full end-to-end RCM or point solutions, we are committed to vitalizing your financial performance so that you can focus on the provider experience and patient care.
